View basket (0 items $0.00)
Error message
- Notice: unserialize(): Error at offset 5 of 154 bytes in variable_initialize() (line 1202 of /home/dh_6hcdc2/yogau.online/docroot/includes/bootstrap.inc).
- The file could not be created.
- The file could not be created.

Yes Men Can Have Pelvic Pain Too
Confession: I treat men for pelvic floor problems. Lots of them. Seriously, I think my schedule is often about 30% men. This shouldn’t have to be a confession. You shouldn’t be surprised by this, but you possibly are. I mean, my female patients are often surprised when they see a male walking out prior to their appointments. I’ve seen that same surprised look on a friend’s (or family member’s, or random person at the bar who happened to ask me what I do for a living’s) face.
For some reason, pelvic floor problems are typically seen as a “woman’s problem,” and this is so unfortunate. It’s unfortunate because it means that many men feel embarrassed or awkward seeking help for a problem seen to be “unmanly.” It’s unfortunate, because so many of the men I treat end up seeing close to five or six physicians, plus two or three physical therapists/chiropractors/acupuncturists, etc. before they actually end up in a place that offers them hope. And it’s unfortunate because it means that many, many men end up suffering from pain for way longer than they should. And this just has to stop.
Pelvic Pain in Men

So, today, we’re going to talk about Pelvic Pain in Men. First, you should know that pelvic pain in men is not that uncommon. In fact, this study estimates that close to 1 in 10 men experience chronic prostatitis/chronic pelvic pain syndrome. Often, pelvic pain is first diagnosed as prostatitis, and I think this happens because of where the pain is located. Prostatitis means inflammation in the prostate, but not all men with the diagnosis actually have inflammation present in the prostate.
I encourage men who are having pelvic pain and receive this diagnosis to ask for a culture. Make sure your prostate is really the one who should be blamed. In some cases, it is (like with bacterial infections). But, oftentimes, these cultures come back negative. So ultimately if the pelvic pain doesn’t go away after a few months, men will often get the diagnosis of chronic nonbacterial prostatitis (which is now categorized as Type 3 chronic prostatitis) or chronic pelvic pain syndrome.
Now you may be thinking, “Jessica, where are you going with all of this?” Well, these men are the ones I generally end up treating. They’ve had pelvic pain for a long time. They haven’t really responded that well to many medications, and still have pretty significant pain levels.
Symptoms of Myofascial Pelvic Pain in Men
-
Pain (which can be sharp, dull, achey, burning, pulling, etc) localized to the lower abdomen, hips, buttock, anus, perineal body, penis, scrotum and/or tailbone.
-
Changes in urination, including urinary urgency/frequency, pain with urination, difficulty starting a urine stream, intermittent or slow urine stream, dribbling after urination and/or urinary leakage.
-
Changes in bowel function including constipation, difficulty emptying bowel movements, pain during and/or after bowel movements.
-
Changes in sexual function including premature ejaculation or erectile dysfunction and/or pain related to sexual function.
What Can a Physical Therapist Do to Help a Man with Pelvic Pain?
Well, a lot. First, you should know that pelvic pain is complicated (I would argue that all pain really is) and when someone has been in pain for a long time, his pain experience becomes multifactorial. We know now that when a person has had pain for a long time, his or her brain changes the way it processes the signals from the area, and many people develop what we call “central sensitization.” This study found that this happens commonly in men with chronic pelvic pain.
Here are some ways to help men experiencing pelvic pain:
-
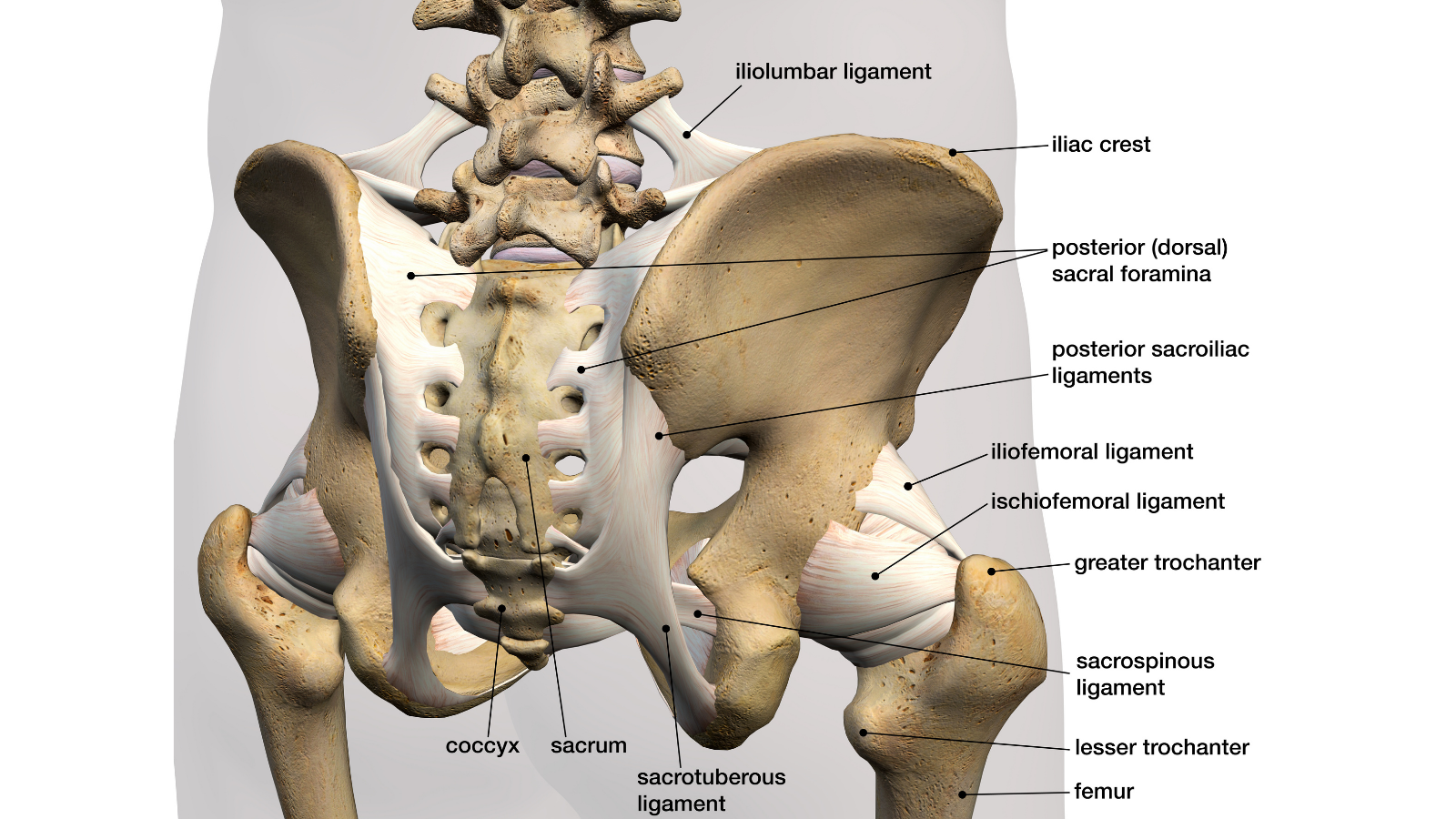
Identification of the musculoskeletal and neuromuscular structures involved: A skilled pelvic PT will perform a comprehensive examination to observe movement patterns and identify structures that could be a component of the pelvic pain experience (including neural, muscular, and connective tissue). For many men with pelvic pain, the pelvic floor muscles can be some of those components. These muscles are actually fairly similar anatomically to the pelvic floor muscles in women (although different, of course!). These muscles can be evaluated externally via palpation or internally via the anal canal. Typically, assessing both ways is the best option as it gives us a comprehensive picture of what is happening from a muscular standpoint.
-
Nervous System (Brain) Training: I could really just stop here because this is our primary and most important goal in physical therapy. Basically, we know that the brain protects a person against “threatening” areas, movements, etc. when a person is experiencing persistent pain. We want to slowly teach the brain that the areas it is protecting are no longer a threat. We want to widen the “safety net” of the brain to allow for more variability in movement. We can do that through manual therapy, down training the nervous system (restoring breathing patterns, guided relaxations, stress management, etc), restorative exercise/movement, and lots of behavioral education.
-
Manual Therapy Techniques: Musculoskeletal structures are often significant components of chronic pelvic pain in men, as I mentioned above. This includes the pelvic floor muscles (both the external, superficial layer of muscles around the penis and perineum as well as the deeper layers of muscle) as well as the muscles around the pelvis (gluteal muscles, adductors, hip flexors, low back muscles, etc.). Many men will also have restrictions in the connective tissue around the pelvis, as well as possibly decreased nerve mobility in some of the nerves around the pelvis. Manual therapy techniques performed both externally and internally help to restore tissue mobility, improve blood flow, and improve the movement of the spine and joints around the pelvis.
-
Improving Bowel, Bladder, and Sexual Habits: As mentioned above, pelvic pain is often accompanied by bladder, bowel or sexual symptoms. Part of helping a client move toward better function means making sure that habits are supporting the best possible outcome. So, we look at everything from dietary habits, toilet positioning, sexual positioning/habits, as well as even sleeping habits to make sure we are addressing as many components of the “pain picture” that we can.
-
Restoring Movement Patterns: Movement patterns are often changed/adapted when a person is experiencing pain. Although this can be a helpful adaptation short-term, these adaptations can often contribute to problems as time goes on. So, our goal is to observe these patterns of movement and identify asymmetries or dominant patterns in order to add some variety to movement and improve the fluidity of movement patterns. Basically, we want to restore the large variety of movement that you used to have before you were dealing with pelvic pain.
-
Much, much more… I know, this is a catch-all subheading. But honestly, there is SO much more that we can do to help someone with pelvic pain depending on the specific case and it would be impossible to get it all in within one blog!
So, basically, what I’m trying to say is that if you’re a man who is having pelvic pain, it’s time to do something about it! I really do recommend seeking out a pelvic PT who is skilled in treating persistent pelvic pain, and comfortable in treating men.
And, if you’re a pelvic PT and don’t feel comfortable treating men? Then, I want you to read what I’m about to write with the kindest, gentlest undertones. It’s time to get comfortable. I’m serious, and I’m talking to you blog reader who only accepts female clients. I understand that some women feel awkward about this, but men need us! They’re hurting, and they need help, so I really think it’s time to get comfortable. Go to a course, seek out mentoring, or whatever you need to get comfortable, but I think we all need to take responsibility to start providing these men with the care they need!
Read more from YogaUOnline and Jessica Reale, PT - Pelvic Floor Problems in the Adult Athlete: Help for Muscle-Related Pain.
Reprinted with permission from jessicarealept.com and now southernpelvichealth.com

Jessica Reale, PT, DPT, WCS is a board-certified specialist in Women’s Health and treats pelvic floor disorders in men, women, and children at One on One Therapy in Atlanta, GA. She received her doctorate in physical therapy (DPT) at Duke University School of Medicine and was the director of the largest pelvic floor rehabilitation program in South Carolina prior to relocating to Atlanta in 2015. Jessica is passionate about helping her patients achieve optimal health through individualized treatment plans integrating the most current research. She is actively involved in educating the community and other professionals and has lectured at support groups, conferences, and universities. Jessica writes regularly about all issues related to pelvic health at her blog, www.jessicarealept.com
Featured Courses