View basket (0 items $0.00)

Study Suggests Yoga Can Help Manage Urinary Incontinence
Urinary incontinence (UI) is a loss of bladder control and is most commonly seen in aged people. While it is a problem in both genders, women experience urinary incontinence twice as often as men. Leakages happen when women exercise, laugh hard, cough, sneeze, or when they are pregnant.
While some individuals experience occasional minor leaks, others wet their clothes frequently. Incontinence is not a disease, but it may indicate an underlying pathological issue that requires intervention. Nearly one-third of women aged 40 years and older experience urinary incontinence, together with associated conditions, including depression, falls, and fractures, social isolation, and physical inactivity.
What Causes Urinary Incontinence?
Urinary incontinence happens when the bladder muscles become too weak or overly active. The bladder is a balloon-shaped, reservoir-like muscular organ that stores and releases urine. It is supported and held in place by the pelvis. The channel that carries urine from the bladder is called the urethra. Ring-like muscles called sphincters help keep the urethra closed so urine doesn't leak from the bladder before you're ready to release it.
Several bodily systems must work together to control the bladder: pelvic floor muscles hold the bladder in place, sphincter muscles keep the urethra closed, the bladder muscle relaxes when urine collects in the bladder and squeezes when it's time to urinate, a set of nerves carry signals from the bladder to the brain know when the bladder is full, and efferent nerves carry signals from the brain to the bladder when it's time to urinate. Urinary incontinence problems occur when any of the above-mentioned features mentioned fail to work optimally.
Types of urinary incontinence include:
-
Stress Incontinence: “Stress" is the pressure on the bladder when an individual coughs, sneezes, laughs or lifts something heavy. If the pelvic and sphincter muscles are strong, they can handle the extra pressure. However, when those muscles get weakened, the sudden pressure pushes urine out of the bladder causing a leak.
-
Urge Incontinence: If you experience involuntary loss of urine after a strong, sudden urge to urinate, you have urge incontinence. Urge incontinence may be caused by a minor condition, such as infection, or a more severe condition, such as nerve damage, a stroke, or an infection.
-
Overflow Incontinence: An individual experiences frequent or constant dribbling of urine due to a bladder that doesn't empty completely.
-
Functional Incontinence: A physical or a mental condition that prevents the individual from reaching the bathroom in time to urinate.
-
Mixed Incontinence: A mix of stress and urge incontinence.
Therapies for Urinary Incontinence
Although a variety of clinical therapies for incontinence are available, many have limitations, particularly for older women who are at the greatest risk of developing this condition. Drugs, including anticholinergic medications, are moderately effective in reducing urge incontinence but are associated with several side effects.
For stress incontinence, surgery is an effective option, but most women do not desire or are not candidates for surgical intervention. Pelvic-floor muscle exercises and bladder training can be highly effective but can be difficult for some women to learn without individualized instruction. Thus, there is a need for effective, alternative treatment that is not only accessible but also well-tolerated by a large number of incontinent individuals.
Yoga can be used to help incontinent individuals to identify and strengthen their pelvic floor muscles without traditional pelvic floor rehabilitation. There are several yoga poses that may be beneficial for improving hip and lumbopelvic stability, mobility, and alignment.
Studies Show Yoga Can Help Manage Urinary Incontinence
Not surprisingly, there are quite a few evidence-based research studies on the management of incontinence with yoga. But I was especially impressed with the rationale and results from one particular study, A group-based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. (1)
Despite the small sample size, the study was published in a peer-reviewed journal, suggesting that the reviewers saw merit in the results. Let me also add that despite being a small pilot study, the results were highly significant with minimal variation between the yoga group and non-yoga group.
The rationale for doing the study was to check the feasibility, efficacy, and safety of yoga therapy for middle-aged and older women with urinary incontinence. The exclusion criteria were stringent and elaborate, and excluded individuals who displayed severe mobility problems or if they had already undergone yoga instruction within the past year, specifically to treat incontinence. Other exclusion criteria included but were not limited to pregnancy within the past six months, ongoing urinary tract infection, neurological issues, including stroke, multiple sclerosis, or Parkinson’s disease, a congenital condition leading to incontinence, fistula in the bladder or rectum, and pelvic cancer or radiation among others.
Women were randomly assigned by a computer to two groups: a yoga group (N=10) and a non-yoga waitlist group (N=9). The non-yoga group received a gift certificate for local yoga studio classes at the end of the study. (I thought this was a novel way to inspire them to do yoga especially after the encouraging results.) The yoga group was enrolled in a six-week yoga therapy program consisting of two group classes/week led by an experienced, certified instructor as well as an assistant and one weekly home practice.
How to Practice Yoga for Pelvic Floor Health
The yoga program, designed by Judith Lasater and Leslie Howard, focused on providing formal instruction and practice in a variety of yoga postures and techniques. The program, which was based primarily on Iyengar yoga, involved a set of eight postures that could be adapted for women of all ages, including those with decreased flexibility or mobility.
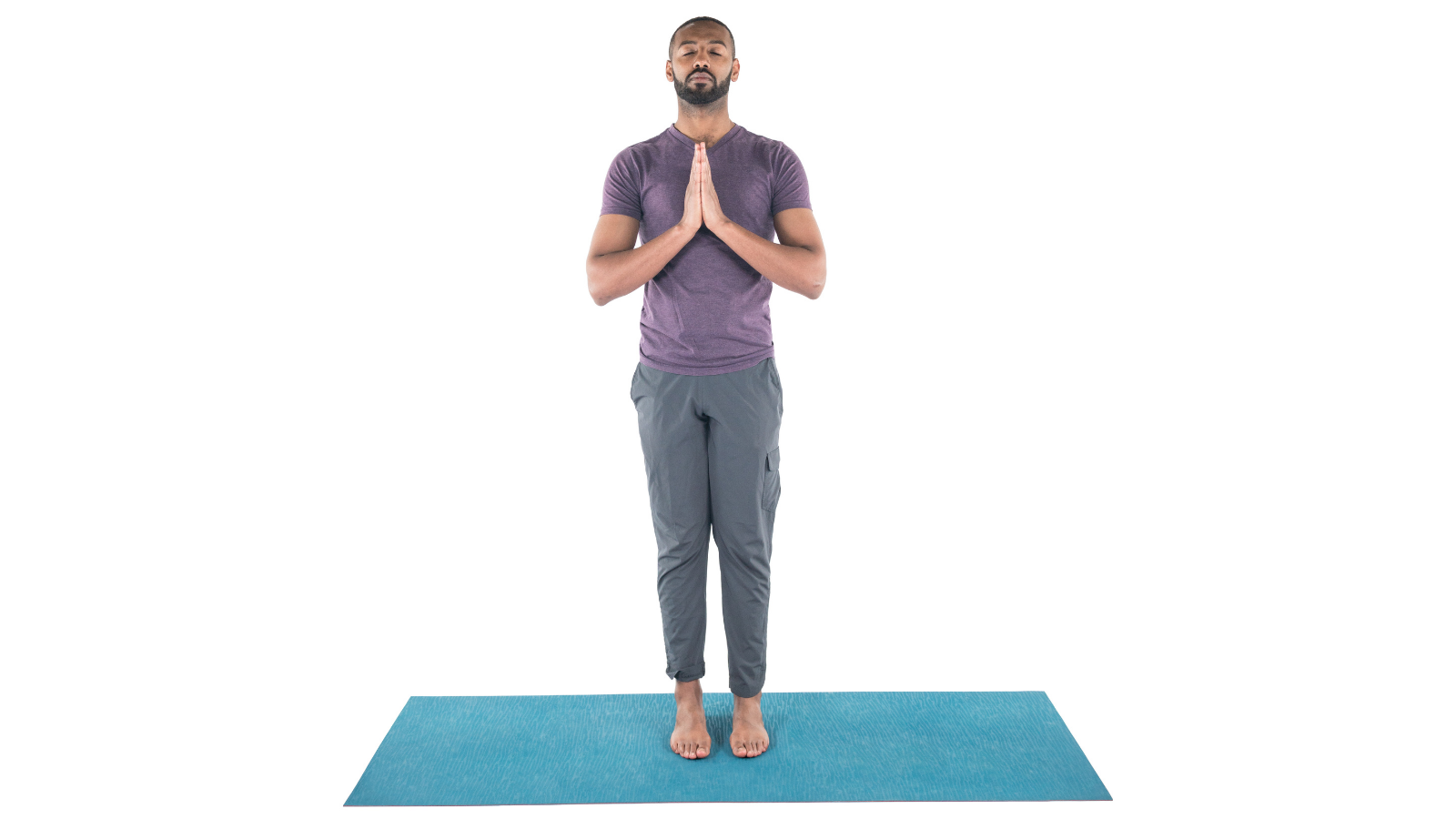
Poses from the study follow. (The exact propping may vary from the photos below.):
-
Mountain Pose (Tadasana)
-
Fierce Pose aka Chair Pose (Utkatasana)

-
Triangle Pose (Trikonasana)

-
Yogic Squatting Pose (Malasana)

-
A variation of Legs Up the Wall Pose (Viparita Karani)

-
Supported Bridge Pose (Salamba Setu Bandhasana)

-
Reclining Bound Angle Pose (Supta Baddha Konasana)

-
Relaxation Pose (Savasana)

Emphasis was laid on strengthening the pelvic floor structures and increasing control over the pelvic floor muscles, in addition to improving general fitness and conditioning; and promoting mindfulness, deep breathing, and relaxation. Participants were also given yoga props and a manual with written descriptions and pictures depicting each of the key yoga postures. Tips were provided on ways to practice each posture safely and comfortably to improve incontinence and pelvic floor function.
The results from the study were quite impressive. The authors noted the following:
-
Teaching women to practice yoga to improve their incontinence was achievable and safe, adherence to group yoga classes and home yoga practice was high, and all the participants were quite successful in learning to practice program-specific yoga postures and techniques.
-
The women who did yoga experienced an overall 70 percent reduction in the frequency of urine leakage, in both total and stress-type incontinence.
-
The positive change was most notably seen in situations involving stress incontinence, urine leakage triggered by activities that increase abdominal pressure, such as coughing or sneezing.
-
Behaviorally, there was significantly greater improvement in the annoyance of their symptoms, compared to non-yoga participants.
While the authors do note that the primary limitations of the study were small sample size and a short duration of yoga practice (six weeks), nevertheless, the study supports the feasibility, efficacy, and safety of yoga therapy to improve urinary incontinence in ambulatory, middle-aged and older women without complicated urologic histories. Since anxiety and depression are often associated with urinary incontinence, the researchers also believe that yoga’s benefits may relate to its emphasis on meditation and relaxation. Additionally, yoga can be practiced by women without continuous or ongoing supervision, thus offering a cost-effective, home-based, self-management strategy for women with incontinence.
Reprinted with permission from Yoga for Healthy Aging.
 Rammohan (Ram) Rao comes from a family of Ayurvedic practitioners and Vedic teachers in India tracing back to the illustrious Vedic-acharya Rishi Kaundinya (although Ram admits he cannot do the Eka pada or Dwi pada Kaundinyasana). With a doctorate in Neuroscience, Ram was a Research Associate Professor at the Buck Institute for Research on Aging. He focused on various aspects of age-associated neurodegenerative diseases with emphasis on Alzheimer’s disease. In addition, Ram completed the academic training at the California College of Ayurveda (CCA) and received his certification as Clinical Ayurvedic Specialist. He has been a faculty member of the California College of Ayurveda and teaches in their Nevada City location. Ram is also a dedicated Hatha yoga practitioner and is a Registered Yoga Teacher from Yoga Alliance USA. In his spare time, he offers consultations in YAMP techniques (Yoga, Ayurveda, Meditation & Pranayama). Ram has published several articles in major Yoga/Ayurveda magazines and has been a featured speaker in several national and international meetings and symposia. He is a member of the National Ayurvedic Medical Association (NAMA) and is on the Research Board of the Association of Ayurvedic Professionals of North America (AAPNA).
Rammohan (Ram) Rao comes from a family of Ayurvedic practitioners and Vedic teachers in India tracing back to the illustrious Vedic-acharya Rishi Kaundinya (although Ram admits he cannot do the Eka pada or Dwi pada Kaundinyasana). With a doctorate in Neuroscience, Ram was a Research Associate Professor at the Buck Institute for Research on Aging. He focused on various aspects of age-associated neurodegenerative diseases with emphasis on Alzheimer’s disease. In addition, Ram completed the academic training at the California College of Ayurveda (CCA) and received his certification as Clinical Ayurvedic Specialist. He has been a faculty member of the California College of Ayurveda and teaches in their Nevada City location. Ram is also a dedicated Hatha yoga practitioner and is a Registered Yoga Teacher from Yoga Alliance USA. In his spare time, he offers consultations in YAMP techniques (Yoga, Ayurveda, Meditation & Pranayama). Ram has published several articles in major Yoga/Ayurveda magazines and has been a featured speaker in several national and international meetings and symposia. He is a member of the National Ayurvedic Medical Association (NAMA) and is on the Research Board of the Association of Ayurvedic Professionals of North America (AAPNA).
References:
Featured Courses