View basket (0 items $0.00)

Healthy You, Healthy Baby: 5 Best Practices for Yoga and Exercise During Pregnancy
I’ll be honest. I’m writing this as much for myself as I am for you. You see, as a women’s health specialist, I have preached the benefits of yoga and exercise during pregnancy for years. I’ve taught classes to women in the community on how to exercise safely and encouraged them in all the way exercise would help their babies, their bodies, their overall health. I’ve lectured other health care professionals on how to help pregnant women start exercise programs, how to monitor them for safety, and which specific exercises are better for women during pregnancy.
But the thing is, I’m now pregnant. 26 weeks to be exact. With this darling, sweet little angel GIRL!

You have to admit, she’s already adorable, isn’t she?
And it has been wonderful, amazing, and incredible to experience—and educational. I thought that I would be the perfect fit, pregnant lady. I would follow all of my own advice on everything and stay super active and fit throughout the pregnancy (I mean, I’ve told so many people that pregnant women can keep exercising at the same level they did before pregnancy!).
But, then reality hit: the first trimester, I was reallllllyyy, realllyyyy tired. Like super tired. In fact, I sometimes just fell asleep on the couch after work (and I am really not a napper). My bedtime effectively became 8:00 pm. And, on top of that, I was nauseated. These things create the perfect combination for not being a super active, fit, pregnant lady. But, I tried to do the best I could, which mostly meant walking sometimes (on the treadmill or outside). Better than nothing though!
Then, the second trimester hit, and all of my symptoms got so much better (just as we tell people they should!). I had more energy, could stay up until at least 9:00 pm, and no longer felt nauseated. But I also was in the process of buying a new house, cleaning and updating said house, then moving, unpacking, and trying to organize our home. So, needless to say, I was not the picture perfect fit, pregnant lady over that time either.
So now we reach today—26 weeks, two weeks away from starting my third trimester. Walking, along with a little bit of yoga/Pilates, is still the best I have done for exercise (Not saying anything bad about walking. I have loved it during pregnancy, it has great benefits, and I plan to continue it! But, I also want to add some variety and a little more frequency to my routine!) So this post serves both to give you some great information, hopefully motivate a few of my fellow pregnant ladies to jumpstart their fitness, and also hopefully to motivate me to up my exercise frequency and throw a little variety in the walking routine.
Why Exercise During Pregnancy?
For many years now, exercise has been considered to be helpful during pregnancy. The benefits of exercise during pregnancy are actually pretty incredible:
-
Cardiovascular benefits (improving blood pressure, heart rate, etc) are passed on from mother to baby, so baby can actually have a healthier little heart when born!
-
Decreased weight gain during pregnancy, which actually can prevent obesity in both mom and baby. Recent studies have suggested that women who gain excessive weight during pregnancy (when starting at normal or overweight BMI) are more likely to have larger babies. When this occurs both mom and baby are at risk for developing obesity in the future.
-
Decreased risk of gestational diabetes (and improvements in women with GDM)
-
Decreased likelihood of Caesarean or operative vaginal delivery
-
Improved postpartum recovery
-
Improved psychological functioning during and after pregnancy
How Should You Exercise During Pregnancy?
The great news is most women can actually continue exercising at the same level they were exercising prior to being pregnant. The American College of Obstetrics and Gynecology just updated their recommendations on exercise during pregnancy this past December. The most recent guidelines recommend that pregnant women exercise 20-30 minutes at moderate intensity most days of the week. The safest types of exercise identified by the committee include:
-
Walking
-
Swimming
-
Stationary cycling
-
Low-impact aerobics
-
Modified yoga
-
Modified Pilates
-
Running or jogging
-
Racquet sports (as long as able to do so maintaining good balance)
-
Strength training
The following types of exercise are recommended to be avoided (for mostly obvious reasons):
-
Contact sports (ice hockey, boxing, soccer, basketball)
-
Activities with a high risk of falling (downhill skiing, waterskiing, surfing, off-road cycling, gymnastics)
-
Scuba diving
-
Skydiving
-
“Hot” yoga or Pilates (due to temperature regulation issues in many pregnant women)
How Hard Should You Exercise?
You may be familiar with the standard method of determining the intensity of exercise by monitoring heart rate. This method is not reliable during pregnancy as cardiovascular function changes during pregnancy, thus the numbers won’t provide accurate guidelines. Instead, women are encouraged to utilize a scale such as the Borg Rate of Perceived Exertion Scale. Basically, this scale goes from 6 (sedentary) to 20 (maximal exertion). Pregnant women are encouraged to aim for moderate intensity—13 to 14 (somewhat hard)—during exercise. Another option for monitoring intensity of exercise is the familiar “talk test.” Basically, as long as you can continue a conversation the intensity is likely not getting overly difficult and should be safe.
When Shouldn’t You Exercise?
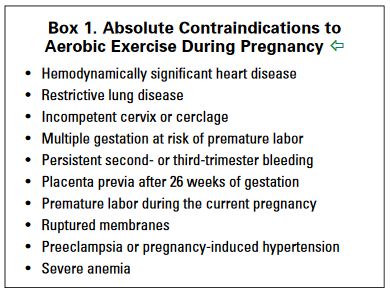
There are several times when it would not be indicated for a pregnant woman to start or continue an exercise program. An absolute contraindication means that if this is occurring, the person should not engage in an exercise program for any reason. Absolute contraindications for exercise are shown in the following table (taken from the recent committee opinion listed above) (1) :
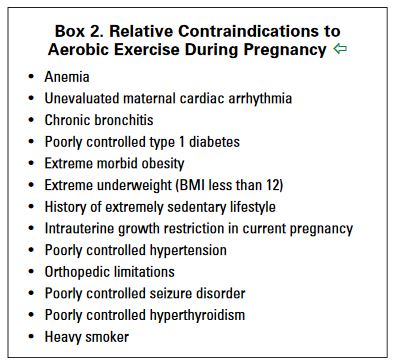
A relative contraindication means that a person should take caution and consult with her physician prior to engaging in exercise. The relative contraindications are listed below (2) :
When Should You Stop Exercising?
There are instances during pregnancy when it may become unsafe to continue an exercise session. If these situations occur, it is important to immediately stop exercising and contact your physician, as continuing to exercise in these scenarios may be harmful to the mother or the baby:
-
Vaginal bleeding
-
Regular painful contractions
-
Amniotic fluid leakage
-
Dyspnea (shortness of breath) before exertion
-
Dizziness
-
Headache
-
Chest pain
-
Muscle weakness impacting balance
-
Calf pain or swelling
Getting Started
If you are pregnant and have not started exercising, it’s really not too late! There are a few things to keep in mind as you get started!
-
Talk to your obstetrician. If exercise is not routine for you, talk to your doctor first before you start a program to make sure it will be safe for you to exercise during your pregnancy.
-
Start gentle and slow. It generally is better to slowly ease into exercise. Remember, the guidelines encourage 20-30 minutes of moderate intensity exercise most days of the week. But, when you first start, it may be wise to start with smaller increments and make 20-30 minutes your goal. Walking, gentle prenatal yoga or water aerobics may be a good, safe place to start.
-
Something is a lot better than nothing. It really is. And I feel ya—some days you’re exhausted or nauseous and just can’t get to the gym. So when that happens, do what you can. Go for a short walk. Try some home prenatal exercise videos. Or, just take the day off and rest. Then try again tomorrow.
-
Listen to your body. And I really mean it. If something isn’t feeling right, pay attention to it! Talk with your doctor if you notice anything unusual or if something isn’t feeling well when you are exercising. Take breaks as you need to, and don’t push yourself too hard.
-
Get some help! Reach out to your local Women’s Health physical therapist to come in for a session and get some help developing a program that will work for you! Also, talk with your physician, midwife or doula about resources in the area. Remember, you don’t have to do this alone!
Study with Sue Elkind and YogaUOnline - Prenatal Yoga Essentials for a Healthy Pregnancy & Birth.
Reprinted with permission from jessicarealept.com

Jessica Reale, PT, DPT, WCS is a board-certified specialist in Women’s Health and treats pelvic floor disorders in men, women, and children at One on One Therapy in Atlanta, GA. She received her doctorate in physical therapy (DPT) at Duke University School of Medicine and was the director of the largest pelvic floor rehabilitation program in South Carolina prior to relocating to Atlanta in 2015. Jessica is passionate about helping her patients achieve optimal health through individualized treatment plans integrating the most current research. She is actively involved in educating the community and other professionals and has lectured at support groups, conferences, and universities. Jessica writes regularly about all issues related to pelvic health at her blog, www.jessicarealept.com
Sources
(1.) www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co650.pdf?dmc=1
(2.) www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co650.pdf?dmc=1
Featured Courses